Shocking Photos Reveal What Hemorrhoids Really Looks Like – See The Photos!
Hemorrhoids are a common and often uncomfortable condition, affecting many people at some point in their lives. These natural structures, which are actually blood vessels in the anus, can become problematic when they swell or cause pain. In this article, we’ll take a closer look at what hemorrhoids really looks like we will see some real photos of hemorrhoids, their complications, what causes them, and the different treatment options available to help manage this health problem. (These pictures may be shocking to some people, please be careful!)
 |
| Shocking Photos Reveal What Hemorrhoids Looks Like |
What Are Hemorrhoids?
Hemorrhoids are natural structures found in everyone’s anus, and they’ve been there since birth.
They're not just simple veins; they’re actually blood-filled sacs connected to small arterial and venous vessels.
Usually, there are about 3 to 4 of these structures, which are grouped together like clusters of grapes, attached to the wall of the anus.
In general, we divide hemorrhoids into two categories: internal and external.
Internal hemorrhoids line the anal canal and appear as small, purple cushions, while external hemorrhoids sit just outside the anus.
You typically only see external hemorrhoids when complications occur, such as swelling or pain.
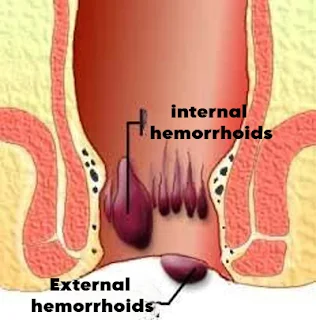 |
| Figure 1: Diagram of Internal and External Hemorrhoids |
Internal hemorrhoids can’t be identified through simple touch. During a consultation, a doctor needs to use a non-invasive tool called an anoscope to examine them.
This device is gently inserted into the anus to allow a clear view of the internal hemorrhoids (see Figure 2).
 |
| Figure 2: View of Internal Hemorrhoids Through an Anoscope |
Complications of Hemorrhoids
Hemorrhoidal Thrombosis
External hemorrhoidal thrombosis is marked by a sudden, painful swelling at the entrance of the anus.
Initially, it can be very painful due to edema (though not always), and then it may turn a bluish color (see Photo 3).
This condition usually resolves on its own within 2 to 3 weeks. The clot may dissolve gradually from the inside, or it can be expelled through a hole in the skin (called a slough), resulting in the clot being discharged and some bleeding (see Photo 4).
The thrombosis can vary in size and may even wrap around the entire anus, a condition known as polythrombosis.
When the external thrombosis no longer appears swollen and is flush with the skin but still causes significant discomfort despite several days of anti-inflammatory treatment, a doctor might perform an incision or excision.
This minor procedure, done in the doctor’s office under local anesthesia, can provide quick relief and help shorten the duration of the flare-up.
Internal Hemorrhoidal Thrombosis
Internal hemorrhoidal thrombosis is less common than external thrombosis but leads to a feeling of tightness and a burning sensation inside the anal canal.
It’s typically more difficult to diagnose, as it can be less noticeable and often requires further examination.
 | ||
| Figure 3: Blueish External Hemorrhoidal Thrombosis (Photo: Dr. V. de Parades) |
 | ||
| Figure 3: Blueish External Hemorrhoidal Thrombosis (Photo: Dr. V. de Parades) |
Bleeding from Hemorrhoids
Because hemorrhoids are a superficial network of blood vessels, one of the most common complications is bleeding.
This bleeding can range from minimal (like a little blood on the toilet paper when wiping) to much more significant (where the toilet bowl is colored or blood drips steadily). This type of bleeding is usually painless and occurs when passing stool.
If the bleeding is heavy and frequent, it can lead to anemia (low red blood cell count) and may require surgical treatment.
Hemorrhoidal Prolapse
Hemorrhoidal prolapse refers to the intermittent or permanent protrusion of internal hemorrhoids outside the anus (also known as prolapsus).
This can happen during bowel movements or when exerting physical effort, like walking for long periods.
The prolapse may either return to its normal position spontaneously or require manual assistance (where the patient presses the hemorrhoids back inside).
Prolapse can also lead to bleeding, itching, and discharge. These symptoms are often chronic, meaning they persist for a long time or even become permanent.
Prolapse usually occurs in adults, especially those suffering from chronic constipation.
Important Reminder!
None of the symptoms mentioned above definitively confirm hemorrhoids as the cause.
Other health conditions affecting the anus or intestines can produce similar signs like pain, bleeding, burning, and prolapse.
That’s why it’s crucial to see a doctor when experiencing chronic symptoms to rule out other potential health issues.
What Triggers or Worsens Hemorrhoids?
There is still some uncertainty about the exact causes of hemorrhoidal disease.
It’s not entirely clear whether the problem is related to blood vessel disease or an issue with the supporting system (anchoring) of the hemorrhoids.
However, several factors are commonly linked to triggering or worsening hemorrhoids, including:
- Intestinal transit problems: Constipation and diarrhea.
- Physical exertion: Heavy lifting, straining, etc.
- Stress
- Irritating medications: Certain laxatives or suppositories.
- Dietary irritants: Spicy foods.
- Menstruation, pregnancy, and childbirth
- Family history: A genetic predisposition to hemorrhoids.
What Treatment Options Are Available for hemorrhoids?
There are three main types of treatments for hemorrhoids:
1. Medications
These are aimed at relieving pain (painkillers or anti-inflammatory drugs), regulating bowel movements (laxatives), improving blood flow (venotonics), reducing swelling and inflammation (suppositories and creams), and protecting the anal canal (ointments and suppositories). Scientific studies support the use of these treatments for managing hemorrhoid flare-ups.
2. Instrumental Treatments
These are performed during a simple consultation with a doctor or surgeon. The goal is to strengthen the support of internal hemorrhoids by creating scar tissue at their base.
The treatments don’t remove the hemorrhoids but help manage symptoms. Some methods include:
- Sclerotherapy (chemical treatment)
- Photocoagulation (thermal treatment)
- Elastic band ligation (placing an elastic band at the hemorrhoid’s base)
These methods are generally well-tolerated since they affect a less sensitive area of the anus.
Complications are rare, affecting fewer than 10% of patients, and mostly involve mild pain and occasional bleeding.
The effects of these treatments often last for at least a year, but repeat sessions might be needed as the symptoms can return over time.
3. Surgical Treatments
In more severe cases, surgery may be required. There are different surgical techniques, such as:
Hemorrhoidectomy (Milligan-Morgan): A complete removal of internal and external hemorrhoids. This procedure is performed under general or spinal anesthesia. Recovery can be painful, requiring 6-8 weeks to fully heal, and it may involve several weeks off work.
Hemorrhoidopexy (Longo technique): This is a “lifting” procedure for internal hemorrhoids using a stapling device. The hemorrhoids are lifted and their blood flow reduced without removal. Recovery is faster than hemorrhoidectomy.
Hemorrhoidal Artery Ligation (HAL): A minimally invasive surgery where small blood vessels feeding the hemorrhoids are tied off using Doppler ultrasound guidance. This technique has quicker recovery times and less pain compared to traditional surgery.
Radiofrequency Ablation: A newer, minimally invasive technique that uses radiofrequency energy to treat hemorrhoidal tissue without making incisions. This method offers good results, but there is still limited long-term data available.
Choosing the Right Treatment
Medications are typically used to relieve acute hemorrhoidal pain and discomfort, especially for external thrombosis or during a flare-up. These treatments are short-term (usually 1-2 weeks).
Instrumental treatments are often used for chronic hemorrhoids, like those causing prolapse or bleeding. Elastic band ligation is particularly effective, though it may cause more discomfort than other methods.
Surgical treatments are generally reserved for severe or advanced cases where other treatments have failed, or for external hemorrhoids that don't respond to non-invasive methods. These options are ideal for patients who want a more permanent solution and are willing to undergo a more extensive recovery period.
 |
| Figure 3: Blueish External Hemorrhoidal Thrombosis (Photo: Dr. V. de Parades) |
Hemorrhoidopexy (or Anopexy) according to Longo
This procedure is a "lifting" of the internal hemorrhoids. Using a mechanical clamp, a collar of mucosa is removed from the top of the internal hemorrhoids, and a mechanical suture is applied using staples.
The hemorrhoids are repositioned but not removed, reducing blood flow while reinforcing the support of the hemorrhoidal tissue in the anus.
This procedure is performed under general anesthesia or spinal anesthesia.
Hemorrhoidal Artery Ligation (HAL)
Hemorrhoidal artery ligation under Doppler control is considered a "mini-invasive" surgery. It involves ligating the blood flow to the internal hemorrhoids.This method is guided by a Doppler probe inserted into the anus. It can be combined with a mucopexy (lifting 1 to 6 points of the anal canal with absorbable thread).
This technique is known as HAL-RAR (Recto-Anal Repair). The recovery is generally less painful, and the return to normal life is faster than with traditional surgery.
Radiofrequency of Hemorrhoidal Packs
Radiofrequency is a recent mini-invasive surgical technique. It treats internal hemorrhoids that bleed and/or prolapse, without causing a wound.It is usually performed under short general or regional anesthesia, often on an outpatient basis.
The technique offers good results with moderate and short-lived pain, but there is still insufficient follow-up to provide reliable data on long-term risks and recurrence rates for hemorrhoid symptoms.
Treatment Choices for Different Situations
Medications can be used for treating acute hemorrhoid pain associated with external thrombosis or hemorrhoidal flare-ups.
These treatments are generally only justified for short periods (usually 1 to 2 weeks).
Instrumental treatments are typically used for internal hemorrhoids that cause chronic symptoms like prolapse or bleeding.
Ligation is slightly more effective than other instrumental methods, but it comes with a bit more pain.
Traditional surgical treatments are usually reserved for cases where instrumental treatments have failed, for very advanced hemorrhoidal diseases, or for external hemorrhoids that do not respond to other treatments.
This is the method to propose to those who are severely bothered by hemorrhoids and want a more radical solution.
Other less invasive techniques can now be offered to people suffering from bleeding and prolapse (internal hemorrhoids) who fear long-term immobilization (due to work) or significant post-operative pain.
